Page Contents
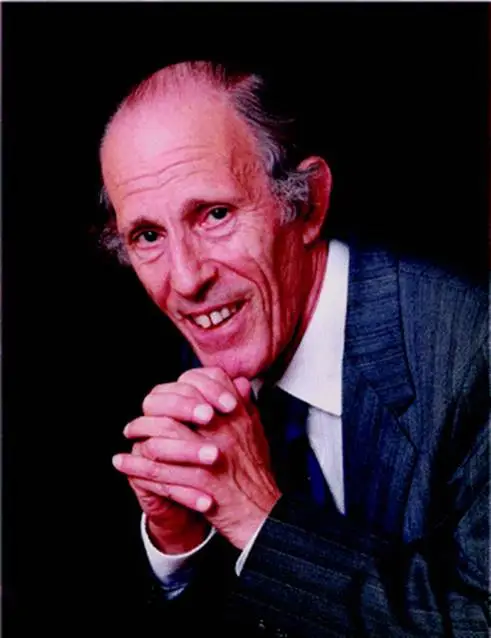
In the 1960s, Professor Bernard Isaacs, a pioneer in geriatric medicine, introduced the concept of the “Geriatric Giants” to describe a group of syndromes that disproportionately affected older adults—immobility, instability (falls), incontinence, and impaired intellect/memory (dementia and delirium). These “giants” symbolised the major threats to independence in ageing populations. They were often interrelated, multifactorial, and rarely confined to a single disease category. Importantly, Isaacs emphasised that these giants were often preventable and treatable, challenging the then-common perception that age-related decline was inevitable and untreatable.
The shift toward Modern Geriatric Giants
Fast forward to today’s ageing societies, and the health challenges of older adults have evolved in both complexity and context. Advances in medicine have prolonged life, but also introduced new burdens: polypharmacy, frailty, sarcopenia, and chronic cognitive decline. The Modern Geriatric Giants framework arose to reflect this shift, emphasising syndromes that are multisystemic, less visible, and rooted in long-term deterioration rather than sudden episodes. They account for modern realities such as polypharmacy from chronic disease management, the rising prevalence of frailty in long-term care, and sarcopenia as a major contributor to falls and immobility. This expanded model recognises that to improve care, we must think beyond symptoms — we must address underlying physiological and systemic decline.
The 5Ms of geriatrics: A practical framework for modern giants
To operationalise the modern approach to geriatrics, clinicians now often use the 5Ms Framework:
Mind
Focuses on cognitive health (e.g., dementia, delirium, depression).
Example: A resident with fluctuating alertness may be experiencing hypoactive delirium due to UTI or anticholinergic medications.Mobility
Encompasses gait, balance, falls, and sarcopenia.
Example: Undiagnosed sarcopenia can lead to recurrent falls and long-term bedbound status in older adults.Medications
Promotes safe prescribing by managing polypharmacy and deprescribing.
Example: A frail older adult on 10 medications including benzodiazepines may experience sedation, leading to falls or confusion.Multi-complexity
Recognises the reality of multiple chronic diseases interacting together.
Example: Diabetes, CKD, and heart failure co-existing in one patient requires a team-based, holistic plan rather than disease-specific care.Matters Most
Puts patient goals, values, and advance care planning at the center.
Example: For a nursing home resident with advanced dementia, the goal may shift from aggressive treatments to comfort-focused care.
This framework is not only a clinical tool but also a philosophical lens for prioritising whole-person care in ageing populations.
Original vs. Modern Geriatric Giants: What’s the difference in philosophy?
The original Geriatric Giants centered on clinical observation and aimed to diagnose and treat specific syndromes. These were ideal for settings where time and diagnostics were limited. In contrast, the modern giants and the 5Ms framework embody a systems-based, anticipatory philosophy. They highlight the importance of interconnectedness between body systems, medications, and care environments, and advocate for interdisciplinary care teams. For example, a fall is no longer seen only as an “instability” issue, it might also reflect sarcopenia, orthostatic hypotension from polypharmacy, or confusion from delirium.
Case study: Modern Geriatric Giants in action
Let’s look at Madam Tan, a 78-year-old nursing home resident who experienced three falls in a month and complained of fatigue and poor appetite. Using Isaacs’ framework, clinicians might focus only on “instability” and “immobility.” However, applying the modern giants and 5Ms, her care team screened her for:
Sarcopenia, confirmed through reduced grip strength and walking speed
Polypharmacy, including sedatives that impaired balance
Frailty, with a Clinical Frailty Score of 6
Mind, detecting signs of mild cognitive impairment
What Matters Most, discovering her wish to stay mobile enough to attend her granddaughter’s wedding

After deprescribing, adding resistance training and protein-rich supplementation, and initiating a multidisciplinary fall prevention plan, Madam Tan regained confidence and mobility. Her falls stopped. Her dignity was restored — not by treating a “fall,” but by managing the systemic roots of her decline.
Conclusion
The original and modern Geriatric Giants each play a crucial, complementary role in understanding and managing age-related decline. Isaacs’ giants still offer timeless clinical relevance for screening and bedside recognition, especially in acute settings. Yet in today’s complex, chronic-care landscape, the modern giants and the 5Ms provide a more dynamic, person-centered, and anticipatory model. Integrating both lenses ensures we can respond not only to what is happening in front of us, but also to what might happen next. For ageing populations to thrive, geriatric care must remain both rooted in tradition and responsive to change.
