Page Contents
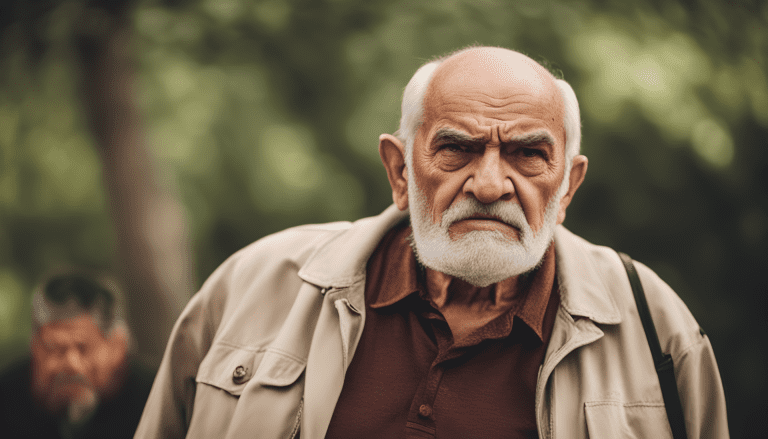
Aggression in elderly individuals with dementia is a deeply challenging and emotionally charged issue faced by caregivers and healthcare professionals alike. These aggressive behaviours, ranging from verbal outbursts to physical violence, are not simply acts of defiance or hostility. Rather, they are often distress signals, rooted in confusion, fear, pain, or frustration. As dementia slowly erodes memory and cognitive function, the ability to express needs or discomfort diminishes, and aggression may become the only available language for someone trying to be heard or understood.
Statistics and trends
Globally, more than 55 million people live with dementia, with nearly 10 million new cases added each year, according to the World Health Organization (2023). In Singapore alone, one in 10 seniors aged 60 and above lives with dementia, a figure projected to rise sharply with a rapidly ageing population.
Studies estimate that up to 80% of individuals with dementia exhibit some form of behavioural and psychological symptoms of dementia (BPSD), with 20% to 40% showing aggression at some point during the disease progression. These behaviors often become more pronounced in moderate to severe stages and pose significant challenges for both family and professional caregivers.
Types of aggression
Aggression in dementia does not always manifest in the same way. It can be categorised into several forms:
Verbal aggression, such as shouting, swearing, or making threats.
Physical aggression, including hitting, pushing, kicking, or biting.
Sexual aggression, which may present as inappropriate touching or sexual comments.
Passive aggression, where the individual resists care passively, refusing to eat, cooperate, or take medication.
Recognising these different types helps caregivers respond appropriately and tailor interventions to the individual’s needs.
Causes of aggression in elderly with dementia
Aggressive behaviours are often triggered by unmet needs or environmental stressors. Some common causes include:
Pain or physical discomfort, such as infections, constipation, or hunger.
Cognitive decline, leading to misinterpretation of surroundings or actions (e.g., mistaking a caregiver’s help as a threat).
Environmental overstimulation or changes in routine.
Psychological triggers, like depression, anxiety, or paranoia.
Communication breakdown, where the inability to express oneself leads to frustration.

Understanding these root causes is essential in providing compassionate and individualised care.
How caregivers can manage aggression
Managing aggression in dementia requires a blend of empathy, patience, and proactive strategies:
Stay calm and speak in a gentle, reassuring tone; avoid arguing or correcting.
Identify triggers by observing patterns in behaviour, i.e. what happens before the aggression starts?
Create a structured, calming environment with familiar objects and routines.
Use distraction and redirection, gently shifting the person’s attention to a comforting activity.
Ensure basic needs are met, including pain management, toileting, hydration, nutrition.
Use validation therapy, affirming feelings rather than challenging false beliefs.
Caregiver education and support are equally critical, training in de-escalation techniques and access to professional help can dramatically improve outcomes.
A systemic and holistic view
Aggression in dementia is not just a behavioural issue, it reflects the broader need for person-centered care. Cultural sensitivity, especially in multicultural caregiving settings, is vital to ensure respect and dignity. Ethical considerations must also be addressed, i.e. the use of restraints or medication should always be a last resort and monitored closely. Additionally, support for caregivers through respite services, support groups, and mental health resources cannot be overstated. Their well-being directly impacts the quality of care provided.

Conclusion
Aggression in dementia is not a choice, it is a symptom. It calls on us to look deeper, to see the person behind the behaviour, and to meet them with understanding instead of judgment.
Caregivers, both formal and informal, need support, empathy, and tools to cope, not blame. By fostering a culture of compassion, education, and person-centered care, we can ease the journey for both the elderly and those who walk beside them. In the end, what matters most is not to “manage” behaviors, but to nurture the humanity that still shines, however dimly, through the fog of dementia.
