Page Contents
Ageing is a natural process, often accompanied by an increased dependency on medications to manage chronic conditions and illnesses. As we grow older, our body’s metabolism slows down, organs may become less efficient, and physiological changes can alter how medications are processed. For elderly individuals, medication becomes a critical component of daily life, offering relief and management of symptoms that would otherwise diminish their quality of life. However, with the increased intake of medications comes the need to understand how they interact with something as routine as food. Drug-food compatibility becomes especially important in the elderly due to the cumulative effects of long-term medication use and the body’s altered response to both drugs and nutrients.
Common illnesses and chronic conditions requiring medications
In the elderly population, there are several prevalent chronic illnesses that necessitate the use of long-term medication. These include:
- Hypertension
Often treated with beta-blockers, ACE inhibitors, and diuretics. - Diabetes
Managed with insulin, metformin, or other anti-diabetic medications. - Cardiovascular diseases
Statins, blood thinners, and other cardiovascular drugs are commonly prescribed. - Osteoporosis
Treated with calcium supplements, bisphosphonates, and vitamin D. - Arthritis and pain management
Involves nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and disease-modifying antirheumatic drugs (DMARDs). - Cognitive decline and dementia: Medications such as cholinesterase inhibitors (e.g., donepezil) and memantine are prescribed to manage symptoms.
With these conditions often requiring the long-term use of medications, the interaction between drugs and food becomes crucial for their effectiveness and to prevent adverse effects.
Drug-food compatibility (or incompatibility)
Drug-food compatibility refers to the way certain foods can affect the absorption, metabolism, and effectiveness of medications. This issue becomes particularly relevant in elderly individuals due to polypharmacy (the use of multiple medications), which can increase the risk of interactions. Furthermore, age-related changes in the digestive system may also exacerbate these interactions.

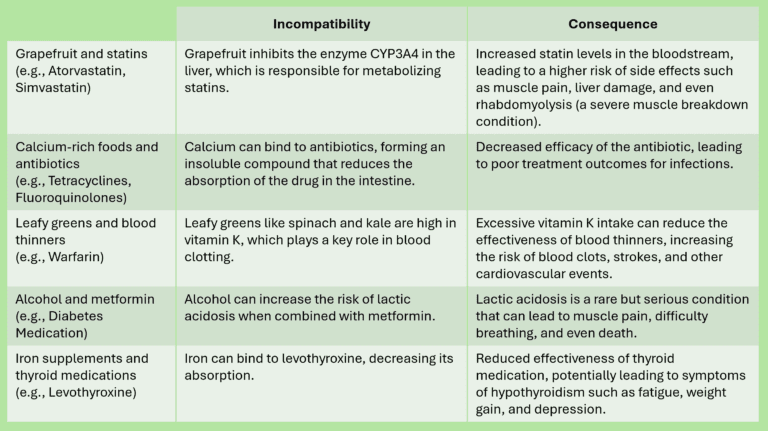
Common incompatibilities between drugs and foods
Specific drug-food interactions can have negative effect and safety concerns in the elderly. Examples of common drug-food incompatibility is shown below:
Consequences of drug-food incompatibilities
The potential dangers that arise when certain foods and medications are consumed together. These incompatibilities can result in a range of issues, from diminished drug effectiveness to severe health risks.
Reduced medication efficacy
One of the most common consequences of drug-food incompatibilities is a decrease in how well a medication works. For example, if calcium-rich foods bind to antibiotics, the drug cannot be absorbed properly, leading to a weakened response to treatment. This can prolong illnesses, making infections harder to treat, or allow chronic conditions like hypertension or diabetes to worsen due to inadequate drug action.Toxicity and overdose
Some drug-food interactions increase the level of medication in the bloodstream, leading to toxic effects. For instance, grapefruit inhibits enzymes that break down certain drugs like statins, causing these drugs to accumulate in the body. This can result in serious side effects such as muscle damage, liver toxicity, or even life-threatening conditions like rhabdomyolysis.Unintended side effects
Incompatibilities can also trigger unintended side effects. Foods that interfere with blood thinners, such as vitamin K-rich leafy greens, can reduce the drug’s anticoagulant effect, increasing the risk of blood clots or strokes. On the other hand, alcohol consumption with certain medications like metformin can raise the risk of severe side effects like lactic acidosis, a potentially fatal metabolic disorder.Delayed recovery
When drug-food interactions reduce a medication’s absorption or effectiveness, it can delay recovery from illness or exacerbate symptoms of chronic conditions. For elderly patients, who may already have weakened immune systems or slower healing processes, this can be particularly harmful, leading to longer hospital stays, increased discomfort, and more intensive treatments.Mismanagement of chronic conditions
For chronic diseases like diabetes, cardiovascular disorders, or thyroid dysfunction, improper drug absorption due to food interactions can make it harder to manage these conditions effectively. Over time, this can lead to complications such as poor blood sugar control, uncontrolled blood pressure, or worsened thyroid function.
Avoiding drug-food Incompatibilities
Given the potential dangers of drug-food incompatibilities, it is vital for elderly individuals and their caregivers to be informed about these interactions. Here are some ways to avoid such issues:
- Consult with healthcare providers
Always ask doctors or pharmacists about potential food interactions when a new medication is prescribed. - Follow instructions carefully
If a medication requires you to take it on an empty stomach or avoid certain foods, it’s crucial to adhere to these guidelines. - Monitor nutrient intake
Be mindful of your diet, especially if you are taking medications known to have food interactions (e.g., avoid excessive vitamin K if on blood thinners). - Plan meals around medication schedules
If a food affects how a drug is absorbed, plan meals accordingly to allow for maximum drug efficacy. - Educate caregivers
Caregivers should also be aware of these interactions to ensure they provide appropriate care for elderly patients.
Polypharmacy and its impact

Polypharmacy, the use of multiple medications simultaneously, is common in the elderly due to the coexistence of multiple chronic conditions. This increases the risk of drug-drug and drug-food interactions, making it more challenging to manage compatibility. The more medications an individual takes, the higher the likelihood that some may interact with each other or with food, further complicating treatment. For this reason, regular medication reviews with a healthcare provider are essential, and simplifying medication regimens where possible can reduce the risks associated with polypharmacy.
Conclusion
Understanding drug-food compatibility is crucial for ensuring the safety and effectiveness of medications, particularly in the elderly population who often rely on multiple drugs for chronic conditions. By being aware of common incompatibilities and taking steps to avoid them, elderly individuals and their caregivers can optimise treatment outcomes and prevent harmful side effects.
Additionally, managing polypharmacy through regular consultations with healthcare professionals can help minimise the risk of both drug-drug and drug-food interactions, ensuring better health outcomes for older adults.
