Page Contents
Diabetes mellitus, commonly known as diabetes, it is a chronic metabolic disease that caused by an impairment in sugar processing (by insulin) in the body and thus causing high sugar content circulating in the bloodstream (hyperglycaemia).

What are the different types of diabetes?
There are 2 common types of diabetes.
- Type I Diabetes is an inherited genetic disease whereby the body is not producing insulin. It usually manifests at young age or through family history. (We will not discuss this topic here)
- Type II Diabetes is an acquired disease whereby pancreas loses its insulin production function or having suboptimal insulin production because of various factors. In some cases, the body is unable to utilise insulin effectively.
Other types of diabetes include Type 3c Diabetes, Maturity Onset Diabetes of the Young (MODY), Latent Autoimmune Diabetes in Adults (LADA), gestational diabetes, cystic fibrosis diabetes, neonatal diabetes, Alström Syndrome, Wolfram Syndrome, steroid-induced diabetes, and prediabetes.
What are the symptoms of hyperglycaemia?
- Fruity-smelling breath
- Nausea and vomiting
- Shortness of breath
- Hyperventilation
- Rapid heartbeat
- Dry mouth
- Weakness
- Confusion
- Abdominal pain
- Unintentional weight loss
- Increased thirst
- Blurred vision
- Frequent urination
- Slow-healing sores or cuts
- Increased hunger
- Numbness or tingling in the hands or feet
- Headache
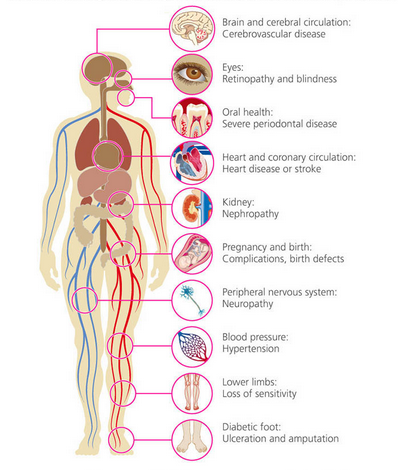
Health implications of diabetes
At first, you would probably have no noticeable discomfort when you have hyperglycaemia, you may have some, but not all the above symptoms, and you assume it is some episodic discomfort due to work stress, diet plan, or extreme weather. Until one day, the symptoms are so overwhelming; you worry and go for a health screening, then you are diagnosed with prediabetes.
- Having mild diabetes, if you follow the medication regime strictly and reduce your weight significantly, you may still achieve partial or complete remission.
- Once your diabetes worsens, you will have to undergo lifetime medical treatment.
- If you leave it untreated, it will eventually lead to complications that damage large and small blood vessels, subsequently lead to:
- diabetic retinopathy – damage of blood capillaries in the retina
- diabetic foot ulcer – open wound resulting from poor circulation and nerve damage
- hypertension – high blood pressure
- nephropathy – deterioration of kidney function
- heart disease – disease which affects the heart
- stroke – interruption of blood supply to the brain
- periodontal disease – gum disease
- cerebrovascular disease – conditions that affect blood flow and blood vessels in the brain
- Over time, diabetes can affect the nerves (neuropathy) and lead to poor blood circulation. Without proper blood circulation, wounds will take longer time to heal, (sometimes it may not even heal). Since there is dysfunction of nerves, you may not feel any pain, and the wound could deteriorate. This is a common condition in diabetic foot ulcer.
- In the long run, without efficient blood circulation, lack of oxygen can cause cells to die, eventually leading to necrosis and amputation.
The good news is that with medical advancement, the risk of most diabetes-related complications can be reduced with early treatment and proper care.
High-risk population
- Obese
- Sedentary lifestyle
- Family history (if a parent or sibling has Type II Diabetes)
- Age (age 45 – 64 were the most diagnosed age group for diabetes)
- Gestational diabetes (female with a history of diabetes during pregnancy)
- High blood pressure (over 140/90 mm Hg)
- High LDL cholesterol and triglyceride levels
Diagnostic & monitoring of diabetes
Regular health screening is important to pick up diabetes-related health problems early. Through screening, you can check your blood pressure, blood glucose levels, HbA1c and cholesterol to make sure they are within recommended ranges.
In clinics, medical professionals will perform haemoglobin A1c test or fructosamine test to accurately measure your blood glucose level.
While for day-to-day monitoring, you have to perform a self-test on fasting blood sugar using a glucometer.
Treatment (for Type II Diabetes)
- Insulin injection (syringe or insulin pen)
- Insulin patch (new treatment technology)
- Oral medications (metformin, sulfonylureas, meglitinides, etc.)
- Pancreas transplant
- Gastric bypass surgery (treatment for obesity)
Living with Diabetes
If you have Type II Diabetes, there are only 2 things you have to watch out:
- Weight
Keep your body weight low and well under control. The heavier you are, the higher risk of you getting various complications such as blood circulation, hypertension, foot ulcer, nephropathy, heart diseases. Therefore, diabetic should workout more to reduce weight and burn out the glucose is your body. - Diet
In particular, carbohydrate (sugar) intake. Diabetic should consume food with low glycemic index to delay the breakdown and release of sugar into blood stream. Instead of skipping meals, eat in smaller portions but increased frequency, this will allow your body to digest food slowly but not spiking the glucose level. Food with soluble fibre (whole grains, nuts, lentils, berries, vegetables, citrus fruits) can slow the absorption of sugar and regulate blood sugar levels. Drinking water and maintain hydration is important as well for diabetic, because dehydration can cause blood pressure to fall and the body to secrete stress hormones which may raise blood sugar. It is important to note that sugary water and caffeinated drinks should be avoided.
As diabetic, you may sometimes over-restrict your sugar intake, or a missed/delayed meal can cause hypoglycaemia. It is a condition where the body sugar level drops drastically. It can cause shakiness, cold sweat, seizures, pass out, or even coma. Hence, it is wise to have some sweet stuffs (candy, chewing gums, a pack of sugar sachet, fruits) with you all the time in case of emergency.
Apart from weight and diet monitoring, you have to check your blood glucose level regularly and remember to take your daily medications or insulin injection.
What you can do if there is still time?
While you are still enjoying perfect health now, it is important to monitor your weight, make sure your BMI falls within normal weight (green zone in figure 1). Good ways to reduce or maintain your weight are to exercise regularly, consume a balanced diet and keep hydrating your systems.
Go for health screening every two years if your age is between 40 – 50, and every year if you age above 50. This will ensure you can pick up early signs and symptoms before any major illnesses surface.
If you want to chart your BMI over a period of time, you can print out the worksheet below in A3 size paper, and follow the instruction given.
How to use this chart?
- This chart is plotted using the BMI formula (weight / (height x height). There is no calculation needed.
- Use a ruler to draw a line along your height at Y-axis (height doesn’t change much).
- Use a ruler to slide along the weight at X-axis to see the intersection where the lines cross.
- The intersection is where your current BMI falls on.
