Page Contents
A heart attack, also known as myocardial infarction, occurs when there is an interruption of blood flow to the heart, leading to one or more areas of the heart muscle not getting oxygen and nutrient supplies. The blockage could cause by a build-up of fatty deposits, including cholesterol and other substances, which form a plaque and narrow the wall of heart arteries (atherosclerosis) or block the small blood vessels entirely. Atherosclerosis is the most common cause of a heart attack. A plaque can detach from the wall and form a clot that blocks blood flow. The interrupted blood flow can subsequently damage or destroy part of the heart muscle.
Infection with COVID-19 may also cause acute myocardial injury and chronic damage to the cardiovascular system, resulting in a heart attack.

Statistics and trends
In Singapore, a heart attack is the number two killer after cancer. Men have a higher risk than women. However, women’s risk of heart attack increases after menopause.
Globally, cardiovascular diseases are the leading cause of death that takes 17.9 million lives each year, one-third of the death occurs prematurely in adults under 70 years old.
What are the complications of heart diseases?
Heart attack could lead to many complications, such as
- Arrhythmias: irregular heartbeats, either too fast or too slowly.
- Cardiogenic shock: a person’s blood pressure drops drastically and the heart cannot supply enough blood for the body to work adequately.
- Hypoxaemia: levels of oxygen in the blood become too low because of inefficient blood circulation.
- Pulmonary edema: fluid accumulates in and around the lungs, which reduces the gas exchange efficiently.
- Deep vein thrombosis (DVT): the deep veins of the legs and pelvis develop blood clots that either block or interrupt the flow of blood in the vein.
- Myocardial rupture: damage on the wall of the heart which increases the risk of a heart wall rupture.
- Ventricular aneurysm: bulging in the ventricle (lower heart chambers) after the episode of heart attack.
- Aneurysm: scar tissue builds up on the damaged heart wall that could lead to blood clots, low blood pressure, and abnormal heart rhythms.
- Angina: sudden chest pain because of insufficient oxygen reaching the heart.
- Congestive heart failure: the heart beats weakly, causing a person feeling exhausted and breathless.
- Edema: fluid accumulates in the ankles, feet and legs, leading to swelling.
- Erectile dysfunction: usually caused by a vascular problem but sometimes also because of depression.
- Pericarditis: inflammation and swelling on the lining of the heart called pericardium, it can cause acute chest pain.
Are you at risk of heart attack?
- Age. As you age (men at 45 and above and women at 55 and above), you are more likely to have a heart attack than are younger adults.
- High blood pressure. Long-term high blood pressure can damage arteries that lead to your heart. High blood pressure that occurs with other conditions, such as obesity, high cholesterol or diabetes, increases your risk even more.
- High cholesterol. Elevated level of low-density lipoprotein (LDL) cholesterol is most likely to form plaque and narrow the arteries.
- High triglycerides. Increased level of triglycerides (a type of lipid in the blood) also increases your risk of a heart attack.
- Obesity. Obese individuals require higher blood pressure to circulate more blood to supply oxygen and nutrients to their bodies.
- Diabetes. High level of blood sugar can damage blood vessels and the nerves that control your heart.
- History of preeclampsia. Having preeclampsia during pregnancy causes high blood pressure and increases the lifetime risk of heart disease.
- An autoimmune condition. Having a condition such as rheumatoid arthritis or lupus can increase your risk of a heart attack.
- Family history of heart attacks. If your family (siblings, parents or grandparents) has a history of early heart attacks (by age 55 for males and by age 65 for females), you may have increased risk.
- Sedentary lifestyle. Being inactive contributes to high blood cholesterol levels and obesity, which subsequently increases the risk of heart attack.
- Stress. Stress may lead to high blood pressure, which can pose a risk for heart attack and stroke. Long-term stress can also elevate the levels of cortisol that increase blood cholesterol, triglycerides, blood sugar, and blood pressure.
- Tobacco. If you are a smoker or have prolonged exposure to secondhand smoke, your chance of dying from a heart attack is 2 to 3 times greater than that of a person who does not smoke.
- Drug abuse. Using stimulant drugs, such as cocaine or amphetamines, can trigger a spasm of your coronary arteries that can cause a heart attack.
- Excessive alcohol consumption. Long-term heavy drinking can lead to sustained hypertension, and it is well-studied to be one of the most important risk factors for having a heart attack or a stroke.
What are the symptoms?
As heart is the organ that circulates oxygen-rich blood to the body, and oxygen-poor blood to the lungs, any drastic changes in blood pressure and oxygen level can cause the following symptoms:
- Prolong tightness, pain, or squeezing sensation in your chest
- Pain that radiates from chest to your neck, jaw, arms, shoulders, or back
- Nausea, indigestion, heartburn, or abdominal pain
- Shortness of breath
- Chills and cold sweat
- Fatigue (blood’s oxygen and nutrient supplies are not efficiently transported throughout the body)
- Light-headedness or sudden dizziness (due to low blood pressure)
Different individual may experience various degrees of symptoms. Some people have mild pain; others may have more severe pain. Some people have no obvious symptoms; others may experience sudden cardiac arrest in the first episode.
How is heart diseases diagnosed?
Whenever you experience a recurrent discomfort of the above symptoms, it is advisable to seek medical consultation at the soonest. Doctor will prescribe a series of tests to analyse your heart functions:
- Electrocardiograph (ECG)
- Cardiac enzyme tests
- Chest X-ray
Emergency response for heart attack
If you have a heart attack,
- Call 995 for help
- Take glyceryl trinitrate (GTN) – relaxes blood vessels and increases blood supply to the heart
- Take aspirin – slows and decreases blood clotting
If someone else has a heart attack and collapse,
- Call 995 for help
- Perform CPR and AED
What are the treatments for a heart attack?
1) Thrombolysis
Chemical thrombolysis uses clot-bursting medications (tissue plasminogen activator (tPA) or urokinase) through an intravenous (IV) line or through a long catheter that delivers drugs directly to the site of the blockage. Mechanical thrombolysis uses a machine to break and aspirate a clot. As thrombolysis may increase risks of haemorrhage (bleeding), it is not suitable for patients who have had a recent major bleed, stroke, uncontrolled hypertension, recent surgery, or bleeding disorders.
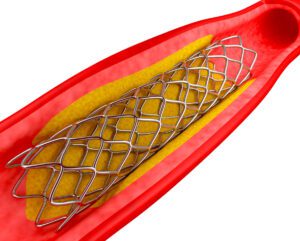
2) Angioplasty
Angioplasty uses a thin wire with a balloon at the end to pass into the blocked coronary artery via a vessel in the groin or arm. The balloon will then be inflated inside the blocked artery to expand and widen it, allowing the blood to flow again. A stent may be permanently placed to keep the vessel wide open.
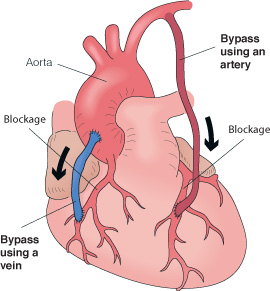
3) Coronary Artery Bypass Graft (CABG)
CABG uses blood vessels from another part of the body and connects them to bypass the blood vessels above and below the narrowed or blocked artery. In the event where more than one heart artery is blocked, CABG could be a better option than angioplasty, that guarantees survival rates.
Living with heart diseases
For people who have had an episode of heart attack, doctors would normally prescribe several kinds of medications to prevent future heart attacks recurrence. These include:
- Aspirin and other anti-platelets
- Beta blockers
- ACE (angiotensin converting enzyme) inhibitors
- Statins
Taking medications can reduce your risk of a recurrent heart attack and help your damaged heart to function better. Follow strictly the medication regimes and commit to regular check-up as advised by your doctor.
What to do if there is still time?
If at this moment you do not have any symptoms of discomfort, there is actually no need to go for ECG check. All you need to do is to ensure you have basic maintenance:
- Healthy lifestyle – manage stress, anger, and have sufficient sleep
- Healthy weight – exercise regularly, and avoid sedentary lifestyle
- Balanced diet – less salt, less oil, less sugar, balanced nutrition and well-hydrated
- Resist smoking, drinking alcohol and taking drugs
- Go for annual health check-up
- If possible, sign up life-saving courses on CPR and AED
