Page Contents
Falls among the elderly are far more common than most people realise. Every year, millions of older adults experience falls, and the consequences can be dire, ranging from diminished quality of life to severe disability and even death.
In previous blog, we have briefly shared an article on falls in the elderly. In this blog, let’s revisit this topic again as it’s crucial to delve deep into the causes of falls to effectively mitigate the risks and enhance the well-being of our seniors.
The impact of falls to an elderly
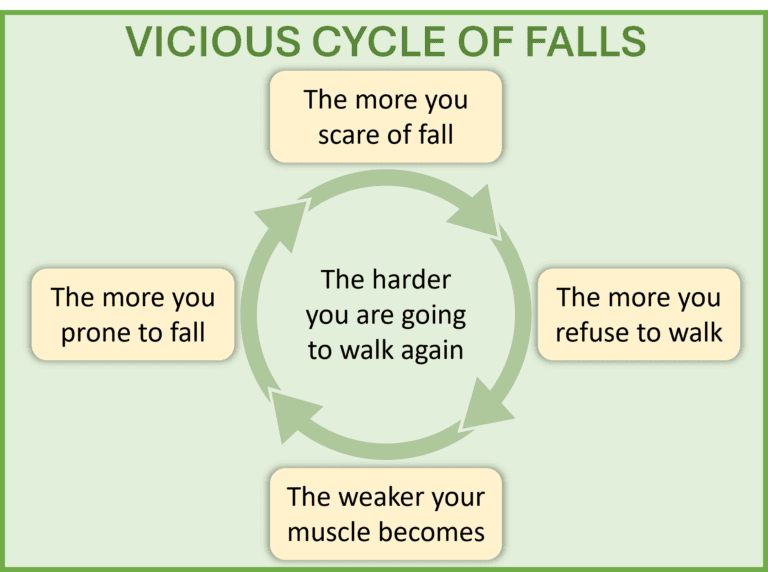
Falls in the elderly aren’t just a matter of stumbling or tripping; they can significantly impact an individual’s overall health and independence. Beyond physical injuries like fractures and sprains, falls can lead to a loss of confidence, increased fear of falling again, social isolation, and depression. Moreover, falls often precipitate a decline in mobility and function, ultimately affecting the individual’s ability to carry out daily activities independently.
Understanding the root causes of falls
Falls among the elderly can stem from various sources, including both intrinsic and extrinsic factors. Let’s delve into some of the common activities and medical conditions that contribute to falls:
Common activities leading to falls
Bending or reaching
Many falls occur when older adults try to pick up objects from the floor or reach for items placed on high shelves, leading to imbalance and loss of stability.

Bathroom rush
Rushing to the toilet, especially during the night, increases the risk of falls due to poor visibility and hurried movements.Transitioning from bed
Getting out of bed, particularly in the morning when muscles may be stiff, poses a significant risk of falls, especially if done too quickly.Standing from squat
Rising from a squatting position can strain muscles and lead to instability, increasing the likelihood of falls.Abrupt turns
Sudden, sharp turns while walking can throw off balance, especially if combined with reduced mobility or strength.
Physical and medical conditions
Muscle weakness
Weak muscles or muscle loss (sarcopenia), particularly in the legs and core, compromise stability and increase the risk of falls.Impaired vision
Poor vision, whether due to age-related changes or eye conditions, makes it difficult to detect obstacles and hazards in the environment.Postural hypotension
Sudden drops in blood pressure upon standing can cause dizziness or lightheadedness, increasing the risk of falls.Neurological disorders
Conditions like Parkinson’s disease, peripheral neuropathy, and stroke can affect balance and coordination, predisposing individuals to falls.Medication side effects
Certain medications, such as sedatives, antidepressants, and antihypertensives, can cause drowsiness, dizziness, or impaired coordination, increasing the likelihood of falls.
Environmental factors
Tripping hazards
Clutter, loose rugs, hanging wire, and uneven flooring increase the risk of tripping and falling.Slippery surfaces
Wet floors, polished tiles, or spilled liquids create slippery surfaces that are particularly hazardous for older adults.Poor lighting
Inadequate lighting, especially in hallways, staircases, and bathrooms, reduces visibility and makes it harder to identify potential hazards.Unstable furniture or bumpy terrain
Unsecured furniture, poorly positioned objects, or uneven surfaces can lead to accidental collisions and falls.

Conclusion
Of course, what are shared above are never comprehensive, yet, it’s imperative to recognise that falls among the elderly are not inevitable and can often be prevented with proper awareness, intervention, and modifications to living environments. By understanding the multifaceted nature of falls – from common activities that lead to them to underlying medical conditions and environmental hazards – we can take proactive steps to reduce the risk and ensure the safety and well-being of our seniors.
Let’s urge older adults to prioritise regular check-ups, maintain an active lifestyle, and make necessary modifications to their homes to create safer living spaces that promote independence and longevity. Together, we can strive towards a future where falls among the elderly are no longer a pervasive threat to their health and quality of life.
