Page Contents
A stroke can happen when the blood vessels or capillaries in the brain are blocked or ruptured, leading to the interruption or reduction of blood supply to part of your brain, causing a cut of oxygen and nutrients to the brain tissue. Within minutes, the brain cells go into shock and die.

Statistics and trends
According to statistics, 15 million people worldwide suffer a stroke every year. Of this population, 1/3 die after stroke and another 1/3 are left permanently disabled. 75% of strokes occur in people at 65 and above, and the remaining people hospitalised for stroke are adults below 65.
In Singapore, stroke has become the fourth most common cause of death after cancer, ischemic heart disease and pneumonia. Even though the incident of stroke rises with ageing, in Singapore, we have seen a decrease in stroke mortality over the years with the developed and organised stroke management system (stroke units) in place.
Are you at risk?
Common conditions with higher risk of getting a stroke.
- High blood pressure – blood pressure above 140/90 can damage blood vessels
- Diabetes – high sugar in the body can make the blood vessels stiff and can also cause a build-up of fatty deposits
- Heart and blood vessel diseases – people suffering damaged heart valves (valvular heart disease) and irregular heartbeat (atrial fibrillation) have a higher risk of stroke
- Obesity and high LDL cholesterol levels – high cholesterol thickens and hardens the arteries
- History of TIA – If you have had one or more TIAs, you are almost 10 times more likely to have a stroke than someone of the same age and sex who has not had a TIA
- High red blood cell count – increase in red blood cells thickens your blood and has a higher chance of getting blood clots
Some unhealthy lifestyles are also more prone to getting stroke.
- Dehydration – insufficient water in the body can lead to thickening of blood
- High salt diet – high salt consumption is associated with hypertension and cardiovascular diseases
- Smoking – smoking doubles your risk of getting ischemic stroke
- Sedentary – inactive lifestyle can lead to obesity, high blood pressure, high cholesterol, and diabetes, which in the long run increases the chances of getting stroke
- Excessive alcohol use – overconsumption can raise your blood pressure, which increases the risk of stroke
- Unhealthy emotions – anxiety, depression, high stress levels
- Sleep deprivation – lack of sleep is associated with increase blood pressure
Of course, there are also some risk factors that are demographic-related such as
- Old age
- Gender
- Race
- Family history and genetics
3 types of strokes
- Ischemic stroke (blockage of a blood vessel)
- Haemorrhagic stroke (sudden bleeding in the brain)
- Transient ischemic attack – TIA (brief blockage, no permanent damage)
What are the symptoms?
Signs and symptoms of a stroke include:
- Numbness or weakness, especially on one side of the body
- Confusion or trouble speaking or understanding speech
- Trouble seeing in one or both eyes
- Trouble walking, dizziness, or loss of balance or coordination
- Severe headache with no known cause
Disabilities after stroke
Our brain is full of blood vessels that supply oxygen and nutrients to the brain cells. As stroke happens in the brain, any deficits in function will depend on which cerebral artery is affected (Figure 1). A typical stroke affects only one hemisphere and the opposite side of your body. In a severe stage, a bilateral stroke affects both sides of the brain and your whole body. A stroke can cause lasting brain damage, long-term disability, and even death if delayed treatment or left untreated.
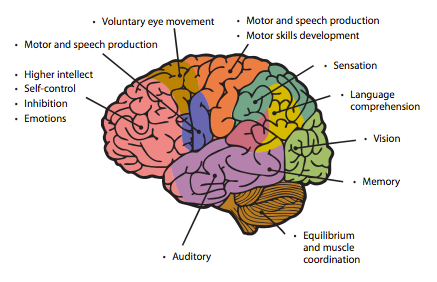
Functional disabilities
- Aphasia or dysphasia – difficulty in finding the right words or understanding what others are saying
- Dysarthria – weakness in the muscles that help speech (dysarthria)
- Dyspraxia – dysfunction of the nerve connection between your brain and mouth, making speaking difficult
- Contractures – permanent shortening or a muscle leading to difficulty with gripping or holding things
- Incontinence – loss of bladder or bowel control
- Pain – caused by actual or potential damage to your tissues (nociceptive pain) or by damage to your nerves that then send incorrect messages to your brain (neuropathic pain)
- Dysphagia – difficulty swallowing or eating. This could also increase the risk of inhaling food or drink into your lungs and cause pneumonia.
- Vision problems – difficulty with visual processing (decreased depth perception and balance), vision loss, blind spot (scotoma), visual neglect, dry eyes, eye movement disorders
- Loss of sensory functions – losing the ability to feel pressure, pain or temperature
- Weakness or paralysis – usually happens on limbs of one side of the body
- Fatigue or tiredness – caused by physical changes, medication, mood changes, depression, anxiety or difficulty in sleeping
Emotional and behavioural changes
- Depression – feeling sad, worthless, difficult to concentrate and self-manage, etc.
- Anxiety – difficult to calm down, feeling worried and frightened
- Easily irritable – reacting aggressively and impulsively on minor discomforts
- Disinhibition – tendency to say and do things that are socially inappropriate
- Apathy – lack of motivation on most things
- Repetitive behaviour – becoming stuck in the repetition of words or behaviours
How to respond?
Apply F.A.S.T. test (Figure 2) if you suspect someone may have a stroke: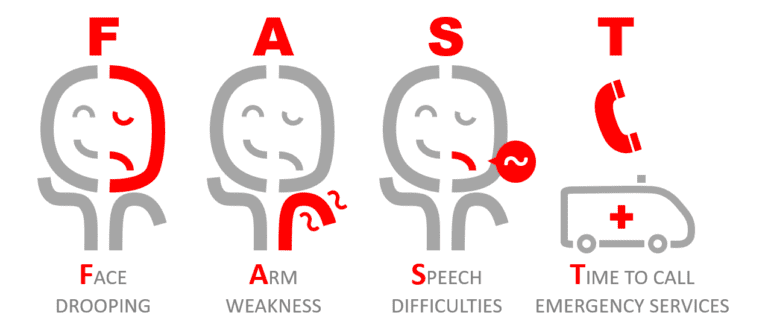
Is stroke curable?
Once warning symptoms are recognised, seek medical help at the earliest possible so that doctors can provide immediate treatment. Only with fast action and early treatment can make a profound difference for your health and recovery.
Treatments for strokes are very specific and depend on the type, size, and location of the stroke in the brain. They may include the use of drugs or surgery to dissolve blood clots or reduce and prevent further haemorrhaging, sometimes emergency surgical intervention may be necessary.
Download a free wallet card here and share it with your friends and family

How is stroke treated?
Treatment for stroke depends on whether it is an ischemic or haemorrhagic stroke, how much time has passed since symptoms began, and whether you have other medical conditions.
Interventions for an ischemic stroke
(or transient ischemic):
- Alteplase / Activase – a recombinant tissue plasminogen activator (tPA)
- Aspirin – blood thinner
- Clopidogrel – antiplatelet
- Balloon angioplasty and stenting procedures
- Using stent retriever
- Aneurysm clipping
- Coil embolisation
- Blood transfusion
- Draining excess fluid
- Surgery or radiation to:
- remove or shrink an arteriovenous malformation (AVM)
- extract pooled blood.
- remove part of the skull temporarily
Life after stroke
After recovery from a stroke, your Activities of Daily Living (ADL) will be greatly affected. You would need to go through a period of rehabilitation and sometimes engage a caregiver. For the rehabilitations, you need to work closely with speech, occupational, and physiotherapists to regain your body’s functions. Very often, you need to have a makeover of your lifestyle to suit your rehabilitation and prevent the next attack.
What you can do if there is still time?
High blood pressure remains the single most important risk factor for stroke. Being able to prevent and diagnose early are critical to reducing the risks significantly.
There are several ways you can improve your lifestyle to reduce your risk of getting stroke:
- Eat a healthy balanced diet and maintain hydrated
- Maintain a normal BMI (Figure 3)
- Exercise regularly
- Have sufficient sleep
- Maintain positive emotions
- Quit smoking
- Limit alcoholic drinks
- Prevent or manage your other health conditions, especially high blood pressure, high cholesterol, diabetes, and obesity
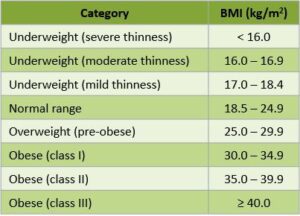
Measuring your BMI
You can key in your weight and height in the calculator and hit the yellow button. Your BMI result will be shown below the calculator.
If you would like to track your BMI, you can visit my blog article on diabetes to download a worksheet and learn how to use it.
