Page Contents
Meals are more than routine in a nursing home. They are the main source of nutrition that supports recovery, strength, and quality of life for elderly residents. Many residents have medical conditions that make eating or swallowing difficult. Providing the right food texture and liquid consistency ensures they eat safely and receive the nutrients they need.
Why do we serve foods and drinks in different textures?
Swallowing problems, known as dysphagia, are common among the elderly due to stroke, dementia, Parkinson’s disease, or frailty. When swallowing is unsafe, food or drink may enter the airway instead of the stomach. Adjusting the texture of food and liquids reduces choking risks and helps residents enjoy meals without fear.

How food texture and liquids are categorised?
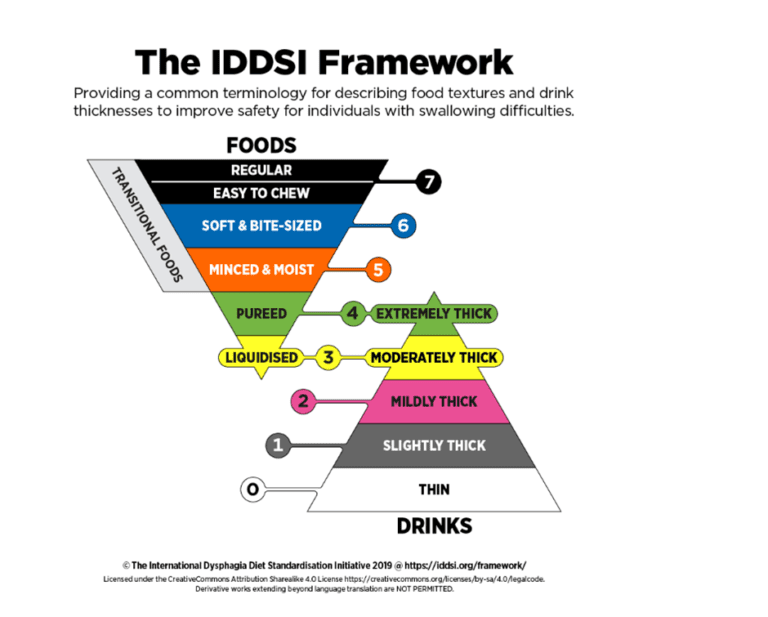
In most nursing homes, textures and consistencies follow international standards such as IDDSI (International Dysphagia Diet Standardisation Initiative). These are the main categories:
-
Food Textures
-
Regular: Normal solid food with no restrictions.
-
Soft & Bite-Sized: Tender foods cut into small pieces, easy to chew.
-
Minced & Moist: Soft, finely chopped foods that form a moist, easily swallowed bolus.
-
Pureed: Smooth, blended foods without lumps, requiring no chewing.
-
Liquidised: Completely smooth, runny foods that need no chewing and minimal swallowing effort.
-
-
Liquids
-
Thin: Regular water or drinks.
-
Slightly Thick: Flows quickly but slightly thicker than water.
-
Mildly Thick: Runs off a spoon but slower, safer for residents with mild swallowing problems.
-
Moderately Thick: Pours slowly, can be eaten with a spoon, safer for more severe dysphagia.
-
Extremely Thick: Stays on the spoon, almost like pudding, for those with very high aspiration risk.
-
What are the dangers of serving the wrong category?
Serving food or drinks that are too thin, hard, or dry for a resident’s swallowing ability is dangerous. The risks may include:
-
Choking leading to airway blockage.
-
Aspiration pneumonia when food or liquid enters the lungs, causing infection.
-
Malnutrition and dehydration if residents avoid eating due to fear of choking.
-
Loss of dignity and quality of life when eating becomes stressful or unsafe.
Assessment before texture modification
Before any changes to food texture or liquid consistency, residents should undergo a swallowing assessment. This is usually done by a speech therapist trained in dysphagia management. The assessment identifies whether a resident is at risk of choking or aspiration and recommends the safest texture. A dietitian may also be involved to ensure that the prescribed texture still provides adequate calories, protein, and hydration. Skipping this step or making assumptions about what the resident needs can result in unsafe feeding and poor nutrition. Every recommendation should be documented clearly and communicated to all staff.
Staff training and monitoring
Once a resident’s diet texture is prescribed, the responsibility shifts to the care team. Staff must be trained to understand the different food textures and liquid consistencies, how to prepare them, and how to recognise when something is incorrect. Mistakes such as serving water to a resident on thickened fluids can have serious consequences. Ongoing monitoring is also essential, as a resident’s swallowing ability may improve with rehabilitation or worsen due to illness. Nurses, caregivers, and kitchen staff should work closely to check consistency, observe residents during meals, and report any changes. A culture of vigilance and teamwork ensures safety.
Conclusion
Providing the right food texture and liquid consistency is not only about safety, but also about preserving nutrition, dignity, and enjoyment of meals. Speech therapists play a central role in identifying the safest textures, while dietitians ensure that modified diets remain balanced and nourishing. Residents should also be included in decisions, choosing flavours and preferred foods within their prescribed diet to maintain appetite and satisfaction. Good practice in nursing homes requires collaboration between professionals, staff training, and resident involvement. When these elements come together, meals become safe, meaningful, and supportive of both health and quality of life.
