Page Contents
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that obstructs airflow and makes breathing difficult. It is especially concerning in older adults, where symptoms are often mistaken for normal ageing. Many elderly individuals live with COPD for years before receiving a diagnosis. Left unmanaged, COPD reduces mobility, increases hospital visits, and shortens lifespan.
Statistics and trends
Globally, COPD is the fourth leading cause of death, according to the World Health Organization. Around 20% of adults over 65 have chronic lung disease, yet many go undiagnosed. In Singapore, respiratory illnesses are among the top ten causes of hospitalisation in the elderly. With ageing populations and increasing urban pollution, the burden of COPD is rising. Despite this, public awareness remains low.
Different types of pulmonary diseases
The major types under COPD include:
- Chronic bronchitis – Persistent cough with mucus for at least 3 months in 2 consecutive years.
- Emphysema – Damage to the air sacs in the lungs, leading to shortness of breath.
- Asthma-COPD overlap – Features of both asthma and COPD in an older adult.
Other age-related lung diseases to monitor include:
- Pulmonary fibrosis
- Bronchiectasis
- Lung infections (e.g. pneumonia, tuberculosis)
Causes and risk factors
The strongest risk factor for COPD is smoking, even if it stopped years earlier. Other contributors include air pollution, exposure to dust or fumes at work, and a history of frequent lung infections, especially in childhood. Ageing naturally reduces lung elasticity and immune function, compounding the risk. A small number of cases are linked to a genetic disorder called alpha-1 antitrypsin deficiency.

Weather is also a contributing factor. Cold or humid conditions can worsen symptoms by increasing airway inflammation and mucus production. Sudden changes in temperature or poor air quality can trigger flare-ups.
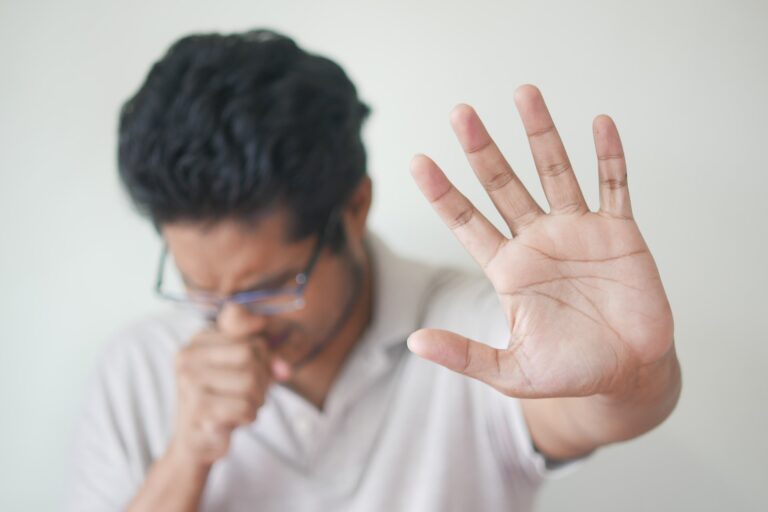
Signs and symptoms of COPD
Common symptoms include chronic cough, shortness of breath, wheezing, and frequent chest infections. Many elderly people also feel fatigued or notice a decline in activity tolerance. In advanced cases, weight loss and low oxygen levels may occur. Because symptoms progress slowly, they are often dismissed until the disease has become severe.
Treatment options for COPD
While COPD is not curable, treatments help maintain function and reduce symptoms.
Inhalers: Bronchodilators and corticosteroids to open airways
Pulmonary rehabilitation: Exercise, education, and breathing strategies
Oxygen therapy: For advanced cases with low oxygen levels
Vaccinations: Influenza and pneumococcal vaccines to prevent complications
Nutrition support: Malnutrition worsens COPD outcomes
Psychosocial support: Anxiety and depression are common in chronic illness
How to prevent COPD?
Prevention and early detection reduce disease burden:
Quit smoking and avoid secondhand smoke
Use masks if exposed to dust or chemicals
Improve indoor air quality with ventilation and air purifiers
Exercise regularly to maintain lung function
Monitor chronic cough or breathlessness; seek early evaluation
Get vaccinated against respiratory infections
Maintain good nutrition and manage comorbidities like heart disease or diabetes

Conclusion
COPD is not just a smoker’s disease. It affects many older adults who have never smoked but were exposed to harmful environments over time. Delayed diagnosis leads to avoidable suffering. If you notice persistent cough, breathlessness, or frequent chest infections in an elderly person, take action early. COPD is manageable with the right care. Early intervention means fewer hospital visits, better quality of life, and greater independence.
