Page Contents
A pressure ulcer, also known as a pressure sore, bed sore, or decubitus ulcer, is a type of injury to the skin and underlying tissue that results from prolonged pressure compress on an area of the body.
Pressure ulcer often occurs in individuals who are immobilized for extended periods, such as people with mobility impairments, spinal cord injuries, paralysed, vegetative state, bedridden elderly people, or those who are critically ill. They are caused by a combination of pressure, friction, and shear forces that damage the skin and underlying tissue, leading to open wounds, blisters, or sores.
Pressure ulcer typically develops on bony areas of the body where there is minimal cushioning, such as the heels, hips, tailbone, and elbows. They can be painful and can lead to serious complications, including infection, sepsis, and even death, particularly in older adults or people with weakened immune systems.

Trends and statistics
Pressure ulcer is generally considered to be a common problem among people with limited mobility or those who spend long periods of time in bed or on wheelchair.
In the United States, the prevalence of pressure ulcers among hospitalised patients ranges from 8.5% to 23.9%, depending on the type of facility and patient population. Among long-term care residents, the prevalence of pressure ulcers ranges from 2.3% to 28%, with higher rates reported among individuals with certain risk factors such as advanced age, malnutrition, and chronic medical conditions.
Globally, pressure ulcers are estimated to affect approximately 1.3 to 3 million young and old people annually, with higher rates reported in developing countries where access to medical care and resources is limited.
Classifications of pressure ulcer
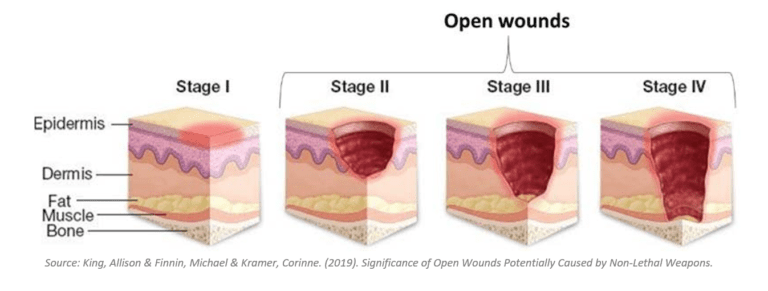
Pressure ulcers are classified based on their severity and depth of tissue involvement, using the staging system developed by the National Pressure Ulcer Advisory Panel (NPUAP). The four stages of pressure ulcers are described below (Figure 1).
- Stage 1
A non-blanchable redness of the skin that does not disappear when pressure is relieved. The affected area may feel warm or cooler than surrounding tissue, and may be painful or itchy. - Stage 2
A partial-thickness of skin loss involving the epidermis (outermost layer of skin) and sometimes the dermis (deeper layer of skin). The wound is shallow and presents as a blister, abrasion, or shallow crater. - Stage 3
A full-thickness of skin loss involving damage or necrosis (death of tissue) of subcutaneous tissue (tissue below the skin) that may extend down to the underlying connective tissue (fascia). The wound presents as a deep crater with or without undermining of adjacent tissue. - Stage 4
A full-thickness of skin loss with extensive tissue damage and necrosis that extends through the fascia and may involve muscle, bone, or supporting structures. The wound may appear as a large, deep, open ulcer with exposed bone or muscle.
In addition to these stages, there is also an “unstageable” category, which includes wounds where the depth cannot be determined due to the presence of slough or eschar (dead tissue) covering the wound bed. This category may also include deep tissue injury (DTI), which presents as a purple or maroon localized area of discoloured intact skin or blood-filled blister caused by damage to underlying soft tissue from pressure or shear forces.
Complications from pressure ulcer
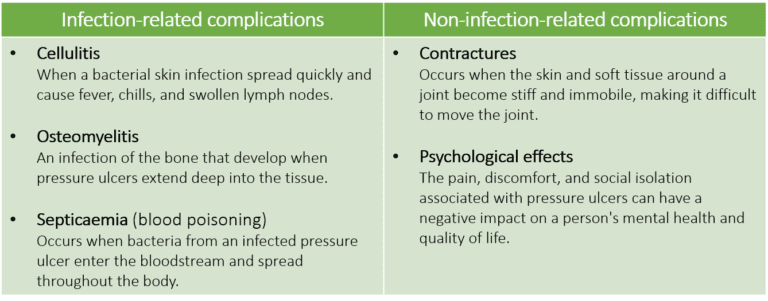
Pressure ulcers can lead to a wide range of complications, some of which can be serious and even life-threatening. The biggest problem with pressure ulcer is infection due to improper wound care. Once infected, it can cause further tissue damage and increase the risk of sepsis (Figure 2).
Risk factors of pressure ulcer
Several risk factors increase your chances of developing pressure ulcers. For example:
- Immobility or limited mobility
People who are bedridden, wheelchair-bound, or have limited mobility for long period. - Malnutrition
Lack of adequate nutrients, especially protein, can impair the body’s ability to heal. - Obesity
Excess weight can exert pressure on bony areas of the body, over time can affect blood flow. - Smoking
Smoking has been correlated with impaired blood circulation and wound healing. - Advanced age
Older adults may have thinner and fragile skin that can be easily damaged by friction and shear forces. - Incontinence
Prolonged exposure to moisture from urine or feces can soften the skin and make it easily tearable. - Chronic medical conditions
Conditions such as diabetes, peripheral vascular disease, and neurological disorders can impair blood flow, reduce sensation, and impair wound healing.
Treatments for pressure ulcer
The treatment of pressure ulcers depends on the severity and depth of the wound. The aims of treatment are to prevent infection, relieve pain, and eventually promote healing. The common mitigation strategies can include:
- Pressure relief
The first step in treating pressure ulcers is to relieve pressure on the affected area. This may involve repositioning or turning the person frequently, or using specialized support surfaces such as breathable mattresses, air cushions, or foam pads. - Wound care
Proper wound care is essential to promote healing and prevent infection. This may involve cleaning the wound with saline solution, removing dead tissue or debris, and applying dressing to protect the wound and promote healing. - Nutrition
Adequate nutrition is equally important for wound healing. This may involve increasing protein and calorie intake, as well as ensuring adequate intake of vitamins, antioxidants, and minerals. - Medications
Medications such as pain relievers, antibiotics, and topical creams may be prescribed to manage pain, prevent infection, and promote wound healing. - Surgery
In some cases, surgery may be necessary to remove dead tissue or repair damaged tissue. - Supportive therapies
Other supportive therapies such as hyperbaric oxygen therapy, electrical stimulation, or ultrasound may be used to promote healing and improve blood flow to the affected area.
How to prevent pressure ulcer?
If you are in the high risk group, but have not developed pressure ulcer, preventing it by maintaining skin integrity and overall health is important. Here are some strategies for preventing pressure ulcers:
- Frequent repositioning
Changing positions frequently can help relieve pressure on vulnerable areas of the skin. It is recommended to reposition every 2 hours for people who are bedridden or immobile. - Use of support surfaces
Support surfaces such as specialized mattresses, cushions, or foam pads can help distribute pressure more evenly and reduce the risk of pressure ulcers. - Good nutrition
Adequate nutrition (protein and vitamins) and hydration are essential for maintaining healthy skin and promoting healing. - Skin care
Keeping the skin clean and dry, using moisturizers, and avoiding excessive exposure to moisture can help prevent skin breakdown. - Management of incontinence
Prompt cleaning and drying of the skin after episodes of incontinence can help maintain skin integrity. - Regular skin assessments
Regular skin assessments can help identify areas of the skin that are at risk of developing pressure ulcers and allow for early intervention.
Conclusion
It is important to identify and treat pressure ulcers early to prevent futher complications from occurring. Regular skin assessments and prompt treatment of pressure ulcers can help prevent tissue damage and reduce the risk of complications.
Education and training for caregivers and family members can help promote good skin care practices and early identification of pressure ulcer development.
Work closely with a healthcare professional to determine the most appropriate treatment plan, as treatment may vary depending on the severity of the wound and the individual’s overall health.
